Making Every Contact Count: Practitioners' Perspectives on Men’s Health Education
A survey of Australian healthcare practitioners highlight the importance of building social, emotional and relational wellbeing into education on engaging with men in care.
Men’s health isn’t just about fixing what’s broken; it’s about understanding what makes men tick. Slowly but surely, we’re seeing a shift toward conversations that dig deeper into men’s social, emotional, and relational wellbeing, because these elements tie into real health outcomes, and men want to talk about these things. Primary care (e.g. general practice) is often the first, and sometimes the only, stop for men seeking help. When practitioners take the time to meet men where they’re at, we start breaking down barriers built by outdated gender norms and other pressures that shape their health journey.
What practitioners are recommending
The Movember Institute of Men’s Health recently asked 126 Australian healthcare practitioners (medical, nursing, pharmacy & allied health disciplines) their appetite for professional education on engaging with men in care. There was a consensus of understanding that men’s health goes way beyond just clinical and biomedical needs; it’s about the bigger picture.
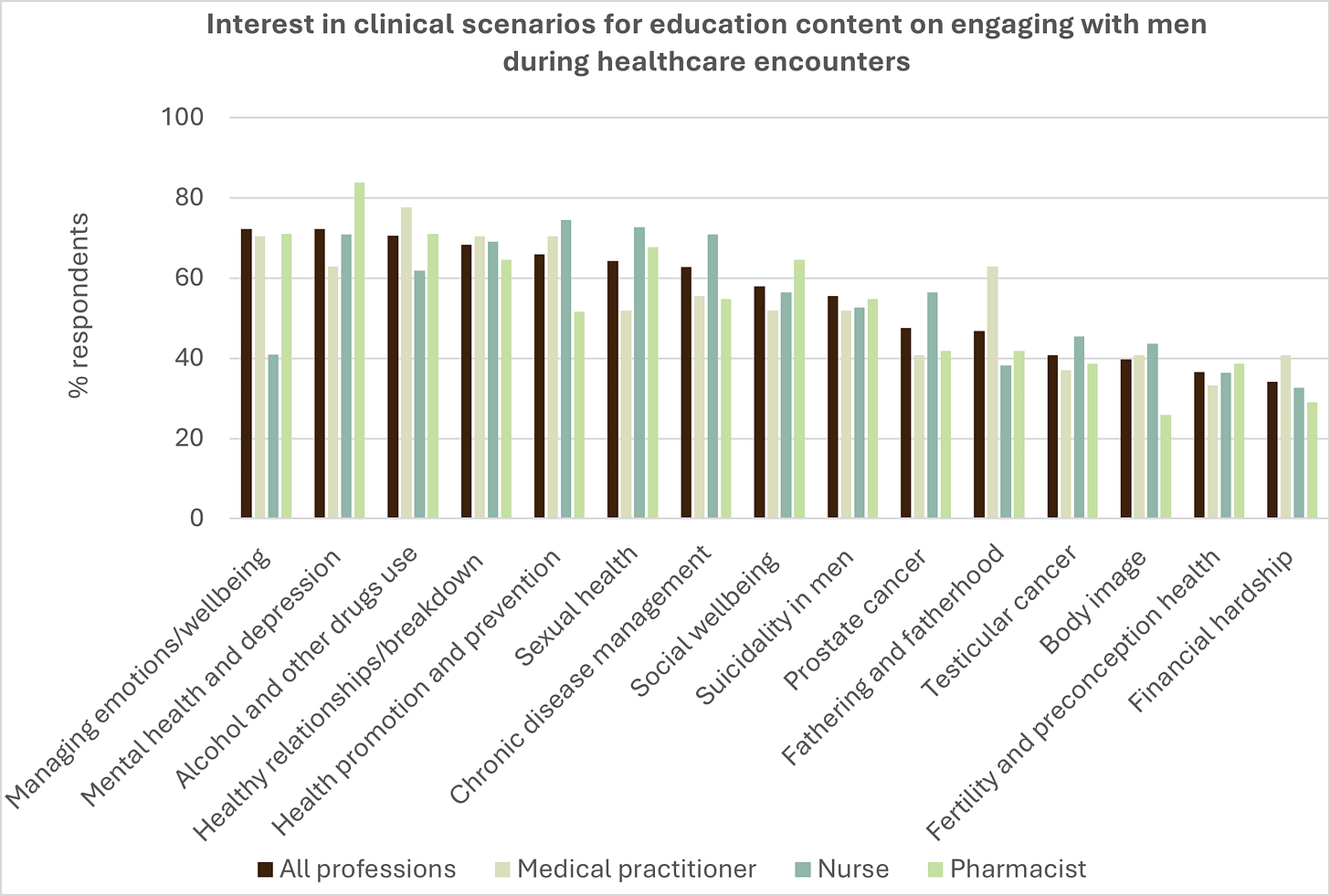
We asked them to pick key scenarios to be used in professional education for healthcare practitioners on approaches to engaging with men in care. Not surprisingly, mental health and depression topped the list (72.2%), as stigma around help-seeking is still leaving too many men struggling in silence. And when they do seek help, too many men are falling through the cracks of a healthcare system that may not be well attuned to their needs. The fallout can be devastating.
Figure: Data from Australian healthcare practitioner insights survey, Movember 2024/25
Reassuringly, the scenario of managing emotions and wellbeing (72.2%), intricately linked to mental health and depression in men, was equally rated in value by practitioners. The other scenarios of interest to 2 in every 3 respondents were alcohol and drug use (70.6%), healthy relationships and breakups (68.3%), and how to effectively engage men in health promotion (65.9%). Notably, when compared to other professions, medical practitioners were more likely to select the social scenario of fathering and fatherhood (63%) (see figure above).
The majority of practitioners were also still interested in the inclusion of scenarios for engaging with men in care on topics of sexual health (64.3%), chronic disease management (62.7%), social wellbeing (57.9%) and suicidality in men (55.6%). Movember’s previous research has found that while reproductive health is commonly covered in university courses and professional education and training programs on men’s health, gender responsive strategies for engaging with men around these and other topics is not covered in curricula. Consistent with this, interest remained in including testicular and prostate cancer as scenarios for education on engaging with men in care.
Men’s mental health: The complexity we need to untangle in care
The survey data have given us a snapshot of how practitioners can engage men in conversations about mental health and emotional wellbeing which doesn’t exist in isolation; it’s tangled up with substance misuse, trauma, relationships, fatherhood, identity and threats to it, and of course physical health. That’s why meeting men in the moment matters.
In particular, relationship struggles can shake a man’s entire foundation. For many, this can lead to emotional distress and, for some, this can catalyse substance misuse, violence, or suicidality. There is an critical opportunity here. By engaging men in discussions around these topics, we are not just empowering them to improve their own wellbeing, we’re setting the stage for healthier families and stronger communities. In this regard, the health system acts as a key domestic violence prevention mechanism.
The power of empathy in healthcare
Practitioners know that real conversations matter. But in fast-paced healthcare environments, how do they make them happen? The answer lies in normalising proactive, empathetic and non-judgmental discussions.
Movember research has shown that men want a safe space; somewhere they can open up without fear of judgment. This is how we start dismantling stigma around alcohol and other drugs and behaviors that impact men’s health and the health of those around them. By reframing health and help-seeking, men can see care as an empowering step, rather than a reluctant one.
Strength-based engagement strategies: A game changer
Practitioners are backing strength-based strategies as a must-have tool in their education; 64% said it would be extremely valuable, and 99.2% overall said it would be of value to them.
Strength-based approaches work because they appeal to what often drives many men; self-reliance, resilience, and their roles as providers. Speaking their language makes engagement easier; helping them seek support, adopt healthier habits and tackle challenges without resorting to behaviors that put their health, work and relationships at risk.
And here’s the reality: 75.4% of surveyed practitioners reported working with men who struggle with gendered barriers (those influenced by social gender role norms) at least some of the time or often. Yet only 1 in 4 practitioners felt confident breaking down those barriers. That needs to change to ensure that every contact with men count.
The future of men’s healthcare demands a focus on workforce upskilling
Upskilling practitioners on engaging men effectively responds to what men have told us they want - healthcare conversations that go beyond the basics. They’re looking for practitioners who genuinely ask, listen, and support them. This isn’t just theory, it’s a real demand backed by men themselves.
So, how do we make this happen?
Movember and the Australian Government, as part of the National Men’s Health Strategy 2020–2030, have teamed up to roll out “Men in Mind” practitioner education for all healthcare professionals to support them in navigating the real-world complexity of men’s lives. Specifically it is designed to ensure healthcare providers have the tools, language and strategies to engage with men in ways that are responsive to their healthcare needs and preferences. Men in Mind is already available for mental health practitioners.